ow to treat GERD?
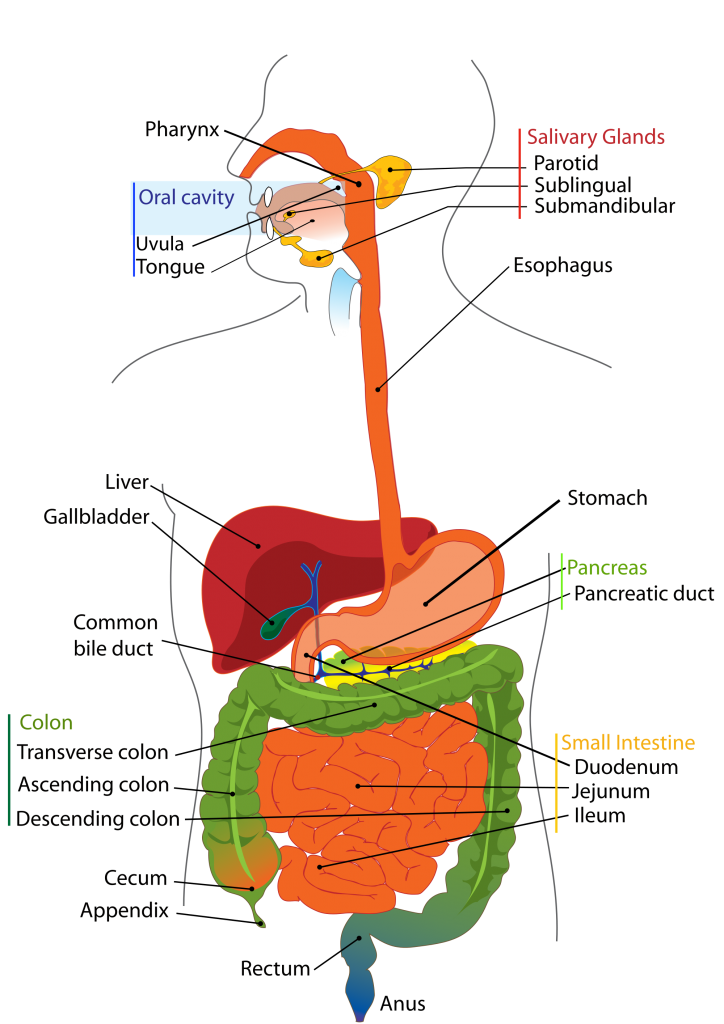
Gastro-esophageal reflux disease (GERD) is one of the most common disorders of the gastrointestinal tract in the Western world(1). The gastro-esophageal reflux disease is defined as the reflux of the stomach’s content back up into the esophagus.
Our stomach makes a powerful brew of hydrochloric acid (HCL) and enzymes (Pepsin, Trypsin, Chymotrypsin) to help break down our food and start the protein digestion process. The pH of this stomach brew is very acidic (pH of 1.0 – 2.5) and could do substantial damage to the esophagus (Esophagitis, Barrett’s Esophagus (BE) and the most feared complication, esophageal adenocarcinoma (2)(EAC = cancer)).
Causes
During normal digestion, the lower Esophageal Sphincter (LES) that separates the esophagus from the stomach opens to allow food to pass into the stomach and closes to prevent food and the acidic stomach brew from flowing back into the esophagus. Gastro-esophageal reflux occurs when the LES is weak or relaxes inappropriately, allowing the stomach’s contents to flow up into the esophagus.
Certain foods and beverages, including chocolate, peppermint, spicy foods, fried or fatty foods, coffee, and alcohol may trigger reflux and heartburn. In addition to fatty foods, smoking, stress and medications could relax the LES too.
GERD may just be an issue of eating in a rushed and/or stressed state and drinking too much liquid during a meal, especially a rushed one. The combination of insufficient stomach acid paired with insufficient magnesium, poor eating hygiene and a food sensitivity is often the perfect storm of factors in chronic GERD.
Some people might suffer from GERD due to a condition called hiatal hernia. Hiatal hernia occurs when the upper part of the stomach moves up into the chest through a small opening in the diaphragm (diaphragmatic hiatus) (3).
Symptoms
The two most typical symptoms are heartburn and regurgitation of the stomach content back into the throat (1). Many people say it feels like food is coming back into the mouth leaving an acid or bitter taste.
When stomach juices bubble up into the esophagus where there is insufficient mucus protection from acidic juices, it hurts. Pepsin can erode tissue but also directly cause an inflammatory response.
Treatment
Decreasing the amount of reflux and reducing the damage to the esophagus, through dietary and lifestyle changes is recommended. In addition, avoiding foods that can weaken or relax the LES and irritate and aggravate the stomach and esophagus is often recommended too.
The mainstream treatment of GERD is to prescribe Proton Pump Inhibitors (PPI’s – Nexium®, Prevacid®, Protonix®, Aciphex®, Prilosec®) or over the counter (OTC) antacid drugs (e.g. Pepcid®, Zantac®, Tagamet®) that clears acid from the esophagus, but also lowers the acidity in the stomach. Lowering the acidity in the stomach may result in reduced digestion and nutrient absorption.
PPI’s inhibits an enzyme necessary for acid secretion in the stomach.
Only use the acid blockers for 2 – 6 weeks and take them as a last resort. The good news is that your esophagus grows new cells every 6 weeks. Use the acid blockers to help heal and regrow the esophagus lining but don’t keep taking them. There is a reason that your stomach is that acidic! If the initial phase of the digestion is inadequate (because of reduced acidity in the stomach), nutrients will not be absorbed, the gastrointestinal (GI) tract can become irritated and yeast and other improper flora can grow in the lower bowel (4). If the reflux continues to be an issue, go and see your doctor.
Dietary and lifestyle changes you can implement are the following:
(1) Consume a plant-based diet.
A plant-based diet is low in fat and high in fiber. High fat intake (from meat, egg yolk and high-fat meals) is associated with increased risk of GERD whereas a high fiber intake decreases the risk (1). The LES is supposed to keep the stomach acids and foods that entered the stomach down, but a high-fat diet will relax the LES and causes reflux to happen.
- Other foods that are associated with weakening the LES are: chocolate, peppermint, coffee, tea (oils in the coffee and tannins in the tea) and alcoholic beverages (3).
- Smoking weakens the LES too. Stop smoking will be important for the ones that do smoke.
- In addition, a plant-based diet is high in antioxidants that can cut the risk of EAC in half, while there is no reduction in risk taking vitamin supplements (5). For this reason I recommend to make and add a green drink/juice on a daily basis for the ones that suffer from GERD (make sure to include cabbage, ginger, other greens you like and a lemon or green apple to cut the flavor).
(2) Stop eating three hours before bedtime and avoid laying down within three hours of eating a meal. In addition, don’t eat a meal heavy in protein late in the day (eat your plant-based protein during breakfast or lunch to give it adequate amount of time to digest).
(3) Avoid foods which aggravate the indigestion, such as raw/uncooked onion, cucumbers, radishes, fruit juices, peppers and hot spices. If any of the foods you eat, even the ones not mentioned in this blog post makes your reflux worse, don’t eat them! A great idea is to keep a daily journal while making these dietary and lifestyle changes. Also, avoid drinking hot liquids as this will aggravate the lining of the esophagus.
(4) Eating Hygiene – change your eating habits.
- Eat smaller, more frequent meals. Do not over-extend your stomach or overeat at a meal.
- Relax and chew your food well before swallowing. Digestion starts in the mouth and it’s the only part of the digestive process that you can control! – chew your food to a cream or use a mechanical blade like a blender, food processor, etc. or use hot water to break down the cell walls by making soups, stews, etc.
- Slow down, eat slowly and enjoy your food. Put your fork down between bites to accomplish this.
- Try to reduce stress, especially during a meal. When we eat in a way that doesn’t allow our nervous system to fully relax and move into parasympathetic mode, we literally create less digestive fluids. It’s part of the body’s survival mechanism. We either ask the body to focus and rush and perform (“fight or flight” = our sympathetic nerve system). Or we ask it to take a break and build strength and energy for the future via eating (“rest and digest” = our parasympathetic nerve system). The body cannot do both at once. Witness the diarrhea or nausea many people feel in stressful situations. Communicate to your body with your actions that it’s safe to relax and let down your guard and focus on digestion.
(5) Drink at least eight 8-ounce glasses of water a day. Hydration is important but don’t drink with your meals as that inhibits digestion, it dilutes your gastric juices. Stop drinking water at least 20-30 minutes before your meal and wait until 20-30 minutes after your meal.
- During the healing process, give up regular and decaffeinated coffee, citrus fruits and juices, tomato products and don’t drink any alcohol to avoid irritating the damaged esophageal lining (3).
(6) Get gravity on your side. Elevate the head of your bed 4 to 6 inches. Don’t use extra pillows, because this will not work. They only bend your head vs. keeping your entire body in an angle. Try to sleep on your left side. The esophagus connects to the stomach on the right side, so lying on the left has the esophagus more on top of the stomach.
Avoid straining, bending over and sudden physical exertion because this can cause increased pressure in the abdomen resulting in hiatal hernia. Pregnancy, obesity, coughing and vomiting can also contribute to this condition. If you are overweight or obese, losing weight can make a huge difference. Also, wear loose clothing to avoid any additional pressure on the stomach.
Some other options and supplements you could consider are:
- Cabbage juice
- Slippery Elm
- A probiotic that includes Saccharomyces Boulardii
- L-Glutamine (crucial amino acid, Band-Aid for the gut lining and could help heal and repair the small intestine)
- Carbonated water
References:
- Lancet 2013 Jun 1; 381: 1933-42
- Gastroenterology Clin North Am 2014 Mar,43(1): 1-14
- WebMD Gastro-esophageal Reflux Disease (GERD)
- Signs and Symptoms Analysis from a Functional Perspective, Dicken Weatherby, N.D. ISBN-13: 978-0976136729
- Int. J. Cancer: 87, 750-754 (2000)







Leave A Comment